Insurance Copays During Covid 19

Second anthem s affiliated plans will continue to waive copays coinsurance and deductibles for diagnostic tests for covid 19 and extending this to include waiver of copays coinsurance and deductibles for visits associated with in network covid 19 testing whether the care is received in a doctor s office urgent care center or emergency department.
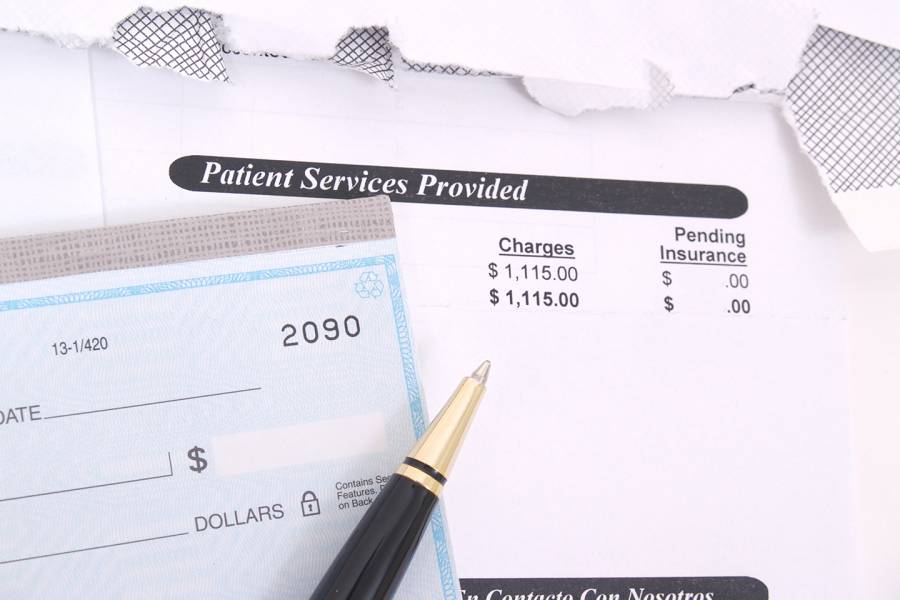
Insurance copays during covid 19. Health care ceo s agree to cover covid 19 treatment waive copays. But this is an emergency he added. We will cover the member responsibility for member copays deductibles or coinsurance costs for covid 19 related services for in network or out of network covered benefits during this time of crisis. Ensuring access to out of network providers for the initial covid 19 test or treatment when no in network providers are available.
The 0 copay applies to services from a network provider and out of network services covered by the plan. Treatment co pays and co insurance. Lab and diagnostic tests radiological and non radiological part b and part d drugs. And removing all cost sharing for telemedicine services including virtual visits with.
Member cost share is not waived for the following services unless they are related to covid 19 testing or treatments. Medicaid will cover the full cost of covid 19 testing for the uninsured as directed by the cares act. Dozens of insurers including aetna cigna and humana. Allways health partners headquartered in massachusetts is removing copays deductibles or coinsurance for testing and copays for treatment at in network facilities.
We will also continue to reimburse providers as we do today consistent with existing contractual arrangements and according to plan benefits in compliance with state and federal rules. Some medicaid health plans on their own are waiving copays related to covid 19 testing and treatment said craig kennedy ceo of medicaid health plans of america.

/cdn.vox-cdn.com/uploads/chorus_asset/file/19783371/1211594075.jpg.jpg)





/cdn.vox-cdn.com/uploads/chorus_image/image/66515347/1207190389.jpg.0.jpg)